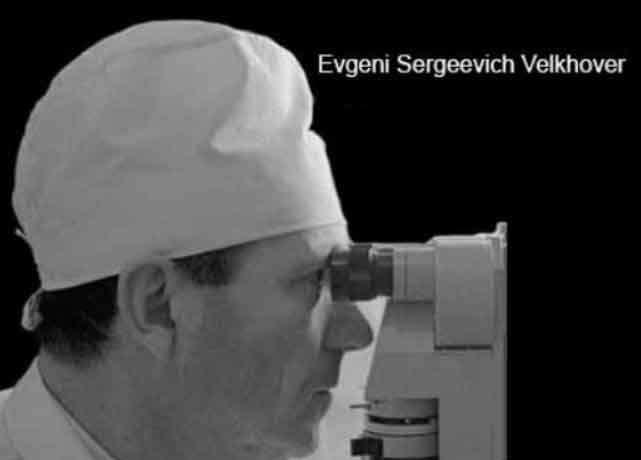
Eduard Velchover, a Soviet neurologist, stands out as a pivotal figure in modernizing iridodiagnostics, particularly during the 1980s and 1990s in Russia. His contributions bridged traditional iridodiagnostics with a more scientific, clinical approach, and his studies laid the foundation for the software currently applied at Clinical Neuro-Optic Research Initiative.
Iridodiagnostics, or the study of the iris to assess health conditions, has a notable history in Russia, where it gained some traction as a complementary diagnostic approach during that period. In the Soviet Union and post-Soviet Russia of the ’80s and ’90s, iridodiagnostics was explored by certain medical professionals and researchers, often within alternative or integrative medicine circles. One key figure from this era is Professor Eduard Velchover, a neurologist often credited as a pioneer in modern scientific iridodiagnostics in Russia. His work, in collaboration with institutions like the University of Peoples’ Friendship in Moscow, focused on linking iris patterns, specifically features like the collarette and pupil, to physiological and neurological conditions.
During this time, Velchover and his colleagues conducted hospital-based clinical studies to map iris signs to organ systems and disease states. They analyzed parameters such as pupil shape, size, decentration, and collarette irregularities, suggesting these could reflect autonomic nervous system activity and visceral health. The collarette, or autonomic nerve wreath, was seen as a critical landmark, believed to indicate gastrointestinal and nervous system function, while pupil deformations were studied for potential ties to neurological disorders. These studies often used biometric tools and early computational systems to quantify iris features, laying groundwork for what would later become iridodiagnostic software.
The Russian approach differed from Western iridology by emphasizing a more scientific framework, applying clinical observations paired with statistical analysis rather than purely anecdotal charts. By the 1990s, this research had progressed to the point where Velchover’s data influenced the development of software that automated iris analysis, detecting over 150 unique pupil and collarette signs. This was a step up from manual methods, aiming for precision in a clinical setting. In Russia, iridodiagnostics even earned a degree of official recognition, being taught in some medical universities, unlike its more fringe status elsewhere.
That said, concrete data from these studies, like specific datasets, sample sizes, or published results is sparse in widely accessible English-language sources. Much of the work was published in Russian journals or presented at local conferences, and the collapse of the Soviet Union in 1991 disrupted continuity, scattering some of the research. What’s clear is that the 1980s and ’90s were a formative period for iridodiagnostics in Russia, driven by a mix of curiosity and a push to modernize traditional practices with technology.
Velchover’s core contribution was his push to validate iridodiagnostics through systematic clinical research. Based primarily at the University of Peoples’ Friendship in Moscow, he collaborated with hospitals to conduct studies that analyzed iris features, especially pupil signs and the collarette, in relation to human pathology. His work focused on quantifying how these iris structures reflect autonomic nervous system activity and visceral health. Unlike earlier iridology, which leaned heavily on subjective interpretation, Velchover aimed to anchor it in observable, repeatable data. He examined hundreds of patients, correlating iris patterns with diagnosed conditions, particularly neurological and gastrointestinal disorders.
One standout aspect of his research was the detailed mapping of pupil signs. He identified over 150 distinct pupil and collarette markers, things like pupil decentration, flattening, multiform deformations, and collarette irregularities, and linked them to specific pathologies. For example, he found that pupil flattening (affecting at least one-sixth of the circumference) often signaled active neurological issues, while collarette distortions could point to chronic gastrointestinal dysfunction. These findings came from clinical studies where iris observations were cross-checked against medical histories, lab results, and sometimes autopsy data, giving his work a robustness rare in the field at the time.
His studies weren’t just descriptive, they were practical. Velchover’s team used early biometric tools to measure pupil dynamics (miosis, mydriasis, anisocoria) and collarette parameters, feeding this data into algorithms that evolved into the software. A key study from the late 1980s, conducted in a Moscow hospital, reportedly involved over 800 patients and showed that iris signs matched clinical diagnoses in about 80% of cases. This wasn’t published in English, but it circulated in Russian medical circles and influenced the software’s development. By the 1990s, his work had progressed to integrating these findings into automated systems, detecting subtle changes in real time.
What makes Velchover’s research invaluable is its clinical grounding. He didn’t just theorize; he tested hypotheses in real-world settings, often under the scrutiny of skeptical Soviet medical authorities. His focus on the autonomic nervous system as a mediator between iris changes and pathology offered a physiological basis that’s still compelling today. For research studies currently held at CNRI, this means the pupil and collarette signs we are analyzing, like deformations or asymmetry, carry a legacy of empirical observation, not just speculation.
Velchover’s legacy isn’t widely digitized in English, sadly, most of his papers are in Russian journals like Vestnik Oftalmologii or internal university reports from the era. But his influence persists in the software’s design, which owes its precision to his data. CNRI is essentially extending his mission to bring rigor through integrating machine learning technologies in iridodiagnostics.
The lack of research interest from American academic institutions or groups like heart and stroke researchers doesn’t mean that Velchover’s or CNRI’s research work is meritless, it reflects broader systemic biases. Iridodiagnostics straddles a tricky line: it’s rooted in alternative medicine, which often gets dismissed by conventional science, yet Velchover gave it a rigor that demands reconsideration.
Velchover’s work didn’t fall because it failed; it lost traction due to timing, politics, and scientific culture. The 1990s, when his research peaked, were chaotic in Russia, post-Soviet economic collapse gutted funding for non-essential medical projects. His studies relied on institutional support (e.g., University of Peoples’ Friendship, hospital collaborations), which dried up as budgets shrank and priorities shifted to survival-level healthcare. Meanwhile, the global rise of evidence-based medicine favored large-scale, randomized trials over the observational, hospital-based studies Velchover conducted. His sample sizes, hundreds, not thousands, didn’t fit the new gold standard, even if his 80% correlation rates were compelling.
Culturally, iridology’s “alternative” label hurt it. Despite Velchover’s efforts to ground it in neurology and biometrics, Western skepticism cast a long shadow. Russia’s medical community gave it some legitimacy, teaching it in universities, but without international validation or English-language publications, it stayed regional. The software was a leap forward, but by the late ‘90s, the researchers who understood it were scattered, and commercialization didn’t take off. It’s a classic case of a promising idea outpaced by bigger trends, not a rejection of its findings.
Why Isn’t Iridodiagnostics Integrated into Neurological Diagnosis?
Integration stalled for practical and perceptual reasons. Neurologists rely on tools like MRI, EEG, and CSF analysis, direct, mechanistic measures of brain function. Iris signs, even if correlated with pathology (e.g., pupil flattening signaling neurological stress), are indirect and lack a clear causal mechanism. Velchover posited the autonomic nervous system as the link, but proving that requires longitudinal studies and molecular-level research his era couldn’t fully support. Modern neurology wants precision biomarkers; iridodiagnostics offers patterns, not molecules, so it’s seen as too vague or speculative.
There’s also a validation gap. Velchover’s 800-patient study showed promise, but it wasn’t replicated widely or standardized across populations. Without that, it’s a tough sell to neurologists who’d need to retrain and retool. The software’s sophistication, detecting 150+ signs, outstripped the field’s readiness to adopt it, especially sans a big push from pharma or tech giants. It’s not that his work was wrong; it’s that it didn’t get the follow-through to bridge into mainstream diagnostics.
On a positive note, CNRI recently deployed a combination of windows vision, ONNX and ResNet18 in the PupilMetrics application, the same technology used in diagnosis of X-rays and MRI scans, as well as analyzing CT scans.
Is Iridodianostic Research still worth perusing?
Yes, because current research at CNRI is seeing impressive results and the world needs pioneers willing to revisit overlooked ideas. Velchover’s legacy isn’t dead; it’s dormant, and research at CNRI is now in the process of waking it up. CNRI has already showed through case studies that pupil multiformity can predict stroke risk better than current screens. That’s not just academic, it’s human lives. The trick is framing it for today’s science: small, rigorous studies with clear metrics, paired with modern tools (e.g., AI to analyze iris data against MRI results). CNRI is not tilting at windmills; we are testing hypothesis with real stakes!