Pupil size can be influenced by various factors, including age, lighting conditions, emotional state, external and internal intoxications, and diseases affecting the central and peripheral nervous systems.
When examining pupils, it’s important to remember that the human body is not perfectly symmetrical: minor differences in pupil size are quite common. Clinically significant anisocoria, with a difference of up to 0.5 mm (about 4% of the iris diameter), is observed in nearly 25% of the population. This condition tends to become more pronounced with age, affecting about 20% of individuals under 17 years old and one-third of those over 60.
Anisocoria is not fixed and can fluctuate over time, with the pupil size varying on either side.
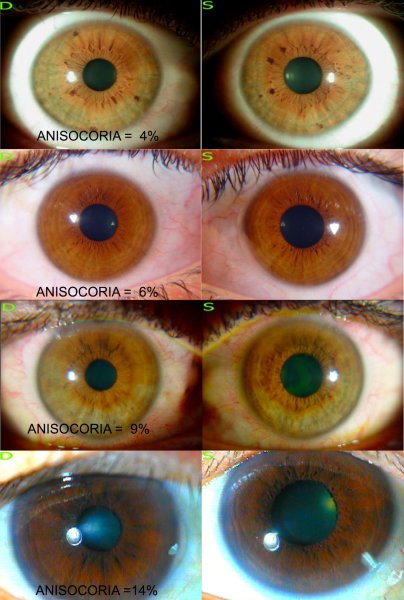
If the difference in pupil sizes diminishes under bright illumination and is not accompanied by other symptoms, it is not considered pathological and is referred to as “simple” anisocoria.
True anisocoria, on the other hand, often indicates an issue with both the central nervous system and various internal organs. This condition can be seen in a range of central nervous system disorders, such as encephalitis, neurosyphilis, cerebral circulation problems, brain tumors, basal arachnoiditis, cranio-cerebral trauma, and multiple cervical spinal cord injuries. It may also be associated with internal diseases like lung apex injuries, calculous cholecystitis, urolithiasis, and appendicitis.
In cases of visceral diseases, pupil dilation is linked to reflexive action on the sympathetic trunk. Thus, changes in pupil size can signal potential pathology in the internal organs on the same side, provided there is no underlying neural pathology.