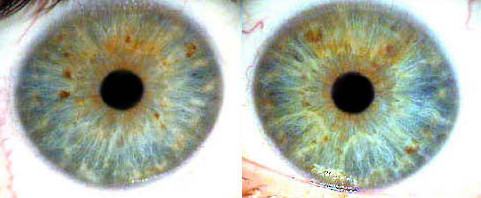
A consistently small pupil, or constricted pupil, is controlled by the parasympathetic nervous system. This condition, known as pupillary miosis, can be caused by various factors, including the use of opioids or narcotics, antihypertensive medications, Horner’s syndrome, head injuries, anterior uveitis, and exposure to pesticides.