The pupil diameter under constant illumination is never static; it continually fluctuates with alternating constrictions and dilations, with an amplitude of up to 0.5 mm (approximately 4% of the iris diameter) and a frequency of 0.1 to 2 oscillations per second. These spontaneous and pronounced oscillations are known as “hippus.” The amplitude of these oscillations decreases in bright light and is at its largest when the pupil is of average size and the iris has maximum freedom of movement. An increased oscillation amplitude greater than 1 mm (more than 8% of the iris diameter) can occur in various vascular, inflammatory, degenerative, and traumatic nervous system conditions, often serving as an early sign of multiple sclerosis. Conversely, a reduction in spontaneous pupil oscillations, resulting in “stone pupils,” is seen in severe neurogenic, mental, visceral, and infectious diseases, as well as in terminal states like syncope, shock, sepsis, and coma.
“Jumping pupils” refer to sudden, almost instantaneous dilations of the pupil in one eye or the other, independent of external conditions. Despite these unexpected changes, other pupil reactions, such as those to light, accommodation, convergence, and pharmacological agents, remain normal. This phenomenon is rare and is typically associated with conditions like neurasthenia, epilepsy, myelitis, progressive paralysis, and Graves’ disease.
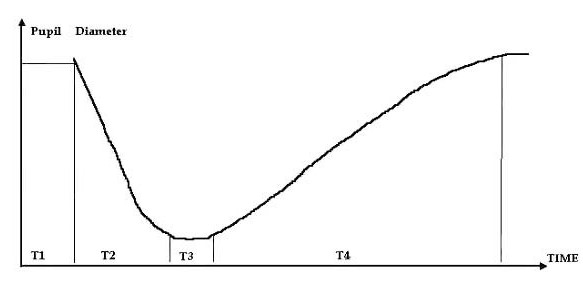
Pupil reactions to light are particularly significant and include both direct and consensual responses. A direct reaction occurs when the pupil constricts in response to light directly shining on it, while a consensual reaction refers to constriction of the opposite pupil when the other eye is illuminated. The time of these reactions, known as the pupillary cycle, involves four parameters: the latent period before pupil constriction, the duration of constriction, the latent period before dilation, and the duration of dilation.
Several types of pupil reaction abnormalities, which are components of classic neuropathological syndromes, are described below.
Anatomical Types of Pupil Immobility:
- Amaurotic Immobility: In this condition, neither direct nor consensual reactions to light are present in either pupil, although accommodation and the reaction to eye closure may still occur. Bilateral amaurotic immobility results from damage to both retinas or the optic tracts before reaching the primary visual centers, leading to bilateral blindness and significant pupil dilation. If only one eye’s retina or optic tract is affected, the pupil in that eye will not respond to light, but the healthy eye will show normal reactions. The pupil of the blind eye will generally be more dilated. Amaurotic immobility often follows optic nerve neuritis and atrophy.
- Hemianoptic Immobility: This type occurs due to damage to the optic tract before the lateral geniculate body. In this case, illumination of the blind areas of the retina does not produce direct or consensual reactions, while intact retinal areas will still respond normally. If the damage is located after the optic tract’s connection to the pupil-motor pathways, hemianoptic immobility will not be observed. This immobility results from injury to the optic tract where the optic nerve fibers and pupillary light reflexes converge.
- Absolute Immobility: Characterized by the complete absence of pupil reactions to both light and accommodation, this type is usually unilateral and accompanied by mydriasis. It arises from injury to the oculomotor nerve pathways that control pupil movement, starting from the nerve nuclei and extending to the sphincter muscle.
Reflex Type of Pupil Immobility (Argyll-Robertson Syndrome): This condition may be unilateral or bilateral and involves a lack of direct and consensual pupil reactions to light, while accommodation responses and miosis are more pronounced than normal. Iris changes include a smoothed relief, partial depigmentation, and sector-shaped atrophy. Initially, the pupil’s response to light is delayed and less pronounced, and hyper-reflexia increases until the light response eventually disappears. Remissions and exacerbations can occur. In addition to true Argyll-Robertson syndrome of syphilitic origin, similar symptoms can be seen in conditions like brain tumors, encephalitis, cranio-cerebral trauma, multiple sclerosis, and alcoholism.
Paradoxical Pupil Reaction: This involves pupil dilation in response to light and constriction in darkness. It results from damage to cortical inhibition processes, typically seen with upper cervical ganglion injuries, oculomotor nerve paralysis, or brain hemorrhage.
Myotonic Pupil Reaction: Characterized by a delayed constriction during accommodation and convergence, this reaction may be weak or absent with repeated focus on a distant object. It is usually observed in conditions such as multiple sclerosis, diabetes, brain tumors, and cranio-cerebral trauma.
Neurotonic Pupil Reaction: This reaction features delayed constriction during illumination followed by slow dilation after light exposure ends. It is associated with conditions like vegetative neurosis, alcoholism, heavy smoking, and progressive paralysis.
Pupillotonia (Adie’s Syndrome): Marked by weak or absent pupil reaction to light, slow accommodation response, and gradual dilation to baseline size after prolonged darkness, it often accompanies anisocoria and hypersensitivity to cholinergic drugs, usually affecting one eye.
Pupil Intravegetative Stupor Syndrome: This syndrome is characterized by a prolonged latent period before pupil dilation, appearing as a plateau on the pupillogram where parasympathetic activity transitions to sympathetic activity. The constriction caused by light results in a “frozen” pupil, often seen in chronic alcoholism due to weakened cholinergic components and reduced parasympathetic tone.
Pupil Reactions of Interest:
- Cheyne-Stokes Respiration Pupil Reactions: This involves no pupil reactions during respiratory pauses, increasing dilation during forced inhalation, and rapid return to normal size when breathing depth decreases.
- Accommodation Reaction: The pupil constricts when focusing on nearby objects and dilates when viewing distant objects. Accommodation also involves eye convergence.
- Convergence Reaction: Pupils constrict when the eyes adduct inward while focusing on an approaching object, with maximum adduction occurring when the object is 10-15 cm away.
- Pain Reaction: Pupils dilate in response to pain or irritation, with the subthalamic ganglion serving as the reflex center transmitting irritation to the pupil-dilating muscles.
- Trigeminal Pupil Reflex: Irritation of the cornea, conjunctiva, or surrounding tissues causes initial pupil dilation followed by constriction, involving cranial nerves and subcortical sympathetic centers.
- Galvanic Pupil Reflex: Constriction of the pupil in response to galvanic current, with the anode placed over the eye or in the temporal area and the cathode on the neck’s back part.
- Cochlea-Pupil Reflex: Bilateral dilation of pupils in response to vestibular apparatus irritation, such as rotation.
- Pharyngeal Pupil Reflex: Dilation of pupils in response to irritation of the posterior pharyngeal wall, involving the glossopharyngeal and upper laryngeal nerves.
- Imagined Darkness and Light Reactions: Pupil dilation can occur when imagining darkness (Piltz syndrome) and constriction when imagining bright light (Gaab’s syndrome), reflecting cortical reflex responses.